FDA is now investigating farms in the Salinas area where the product originated.
https://www.fda.gov/food/outbreaks-foodborne-illness/investigation-e-coli-o157h7-outbreak-linked-romaine-salinas-california-november-2019
Investigation of E. coli O157:H7 Outbreak Linked to Romaine from Salinas, California, November 2019
FDA investigating farms in Salinas, warns against eating romaine lettuce from that area, CDC reports increasing case count
November 26, 2019
Case Counts
Total Illnesses: 67
Hospitalizations: 39
Deaths: 0
Last illness onset: November 14, 2019
States with Cases: AZ (3), CA (4), CO (1), ID (3), IL (1), MD (4), MI (1), MN (3), MT (1), NE (1), NJ (1), NM (2), OH (12), OR (1), PA (3), TX (2), VA (2), WA (1), WI (21)
November 26, 2019
Recommendation
FDA, CDC, and state health authorities are investigating an outbreak of illnesses caused by E. coli O157:H7 in the United States. Epidemiologic, laboratory, and traceback evidence indicates that romaine lettuce from the Salinas, California growing region is a likely source of this outbreak. The CDC is reporting an increase in the case count to 67 and that the most recent illness onset date is November 14, 2019.

Consumers: Consumers should not eat romaine lettuce harvested from Salinas, California. Additionally, consumers should not eat products identified in the recall announced by the USDA on November 21, 2019.
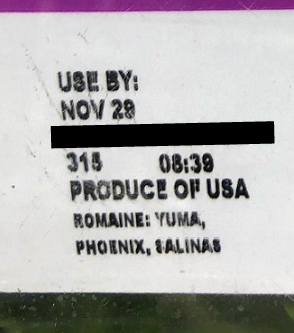
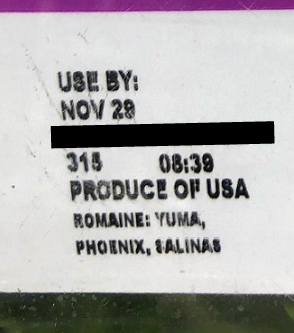
Romaine lettuce may be voluntarily labeled with a harvest region. If this voluntary label indicates that the romaine lettuce was grown in “Salinas” (whether alone or with the name of another location) do not eat it. Throw it away or return it to the place of purchase. If romaine lettuce does not have information about harvest region or does not indicate that it has been grown indoors (i.e., hydroponically- and greenhouse-grown), throw it away or return it to the place of purchase. Consumers ordering salad containing romaine at a restaurant or at a salad bar should ask the staff whether the romaine came from Salinas. If it did, or they do not know, do not eat it.
At this time, romaine lettuce that was harvested outside of the Salinas region has not been implicated in this outbreak investigation. Hydroponically- and greenhouse-grown romaine, which is voluntarily labeled as “indoor grown,” from any region does not appear to be related to the current outbreak. There is no recommendation for consumers to avoid using romaine harvested from these other sources.
Restaurants and Retailers: Restaurants and retailers should not serve or sell romaine harvested from Salinas, California. If you do not know the source of your romaine lettuce, and if you cannot obtain that information from your supplier, you should not serve, nor sell it.
Suppliers and Distributors: Suppliers, distributors and others in the supply chain should not ship or sell romaine harvested in Salinas, California. If the source of the romaine lettuce is unknown, you should not ship, nor sell the product.
For Restaurants, Retailers, Suppliers and Distributors: Currently, the FDA does not have enough traceback information to identify the specific source of the contamination that would allow us to request a targeted recall from specific growers. At this stage in the investigation, the most efficient way to ensure that contaminated romaine is off the market would be for industry to voluntarily withdraw product grown in Salinas, and to withhold distribution of Salinas romaine for the remainder of the growing season in Salinas. FDA has made this request of industry.
At this time, romaine lettuce that was harvested outside of the Salinas region has not been implicated in this outbreak investigation. Hydroponically- and greenhouse-grown romaine, which is voluntarily labeled as “indoor grown,” from any region does not appear to be related to the current outbreak. There is no recommendation for consumers or retailers to avoid using romaine harvested from these other sources.
https://www.fda.gov/food/outbreaks-foodborne-illness/investigation-e-coli-o157h7-outbreak-linked-romaine-salinas-california-november-2019
Investigation of E. coli O157:H7 Outbreak Linked to Romaine from Salinas, California, November 2019
FDA investigating farms in Salinas, warns against eating romaine lettuce from that area, CDC reports increasing case count
November 26, 2019
Case Counts
Total Illnesses: 67
Hospitalizations: 39
Deaths: 0
Last illness onset: November 14, 2019
States with Cases: AZ (3), CA (4), CO (1), ID (3), IL (1), MD (4), MI (1), MN (3), MT (1), NE (1), NJ (1), NM (2), OH (12), OR (1), PA (3), TX (2), VA (2), WA (1), WI (21)
November 26, 2019
Recommendation
FDA, CDC, and state health authorities are investigating an outbreak of illnesses caused by E. coli O157:H7 in the United States. Epidemiologic, laboratory, and traceback evidence indicates that romaine lettuce from the Salinas, California growing region is a likely source of this outbreak. The CDC is reporting an increase in the case count to 67 and that the most recent illness onset date is November 14, 2019.

Consumers: Consumers should not eat romaine lettuce harvested from Salinas, California. Additionally, consumers should not eat products identified in the recall announced by the USDA on November 21, 2019.
Romaine lettuce may be voluntarily labeled with a harvest region. If this voluntary label indicates that the romaine lettuce was grown in “Salinas” (whether alone or with the name of another location) do not eat it. Throw it away or return it to the place of purchase. If romaine lettuce does not have information about harvest region or does not indicate that it has been grown indoors (i.e., hydroponically- and greenhouse-grown), throw it away or return it to the place of purchase. Consumers ordering salad containing romaine at a restaurant or at a salad bar should ask the staff whether the romaine came from Salinas. If it did, or they do not know, do not eat it.
At this time, romaine lettuce that was harvested outside of the Salinas region has not been implicated in this outbreak investigation. Hydroponically- and greenhouse-grown romaine, which is voluntarily labeled as “indoor grown,” from any region does not appear to be related to the current outbreak. There is no recommendation for consumers to avoid using romaine harvested from these other sources.
Restaurants and Retailers: Restaurants and retailers should not serve or sell romaine harvested from Salinas, California. If you do not know the source of your romaine lettuce, and if you cannot obtain that information from your supplier, you should not serve, nor sell it.
Suppliers and Distributors: Suppliers, distributors and others in the supply chain should not ship or sell romaine harvested in Salinas, California. If the source of the romaine lettuce is unknown, you should not ship, nor sell the product.
For Restaurants, Retailers, Suppliers and Distributors: Currently, the FDA does not have enough traceback information to identify the specific source of the contamination that would allow us to request a targeted recall from specific growers. At this stage in the investigation, the most efficient way to ensure that contaminated romaine is off the market would be for industry to voluntarily withdraw product grown in Salinas, and to withhold distribution of Salinas romaine for the remainder of the growing season in Salinas. FDA has made this request of industry.
At this time, romaine lettuce that was harvested outside of the Salinas region has not been implicated in this outbreak investigation. Hydroponically- and greenhouse-grown romaine, which is voluntarily labeled as “indoor grown,” from any region does not appear to be related to the current outbreak. There is no recommendation for consumers or retailers to avoid using romaine harvested from these other sources.
Background
According to the CDC, as of November 25, 2019, 67 people infected with the outbreak strain of E. coli O157:H7 have been reported from 19 states. The case patients report that illnesses started on dates ranging from September 24, 2019 to November 14, 2019.
The Maryland Department of Health identified E. coli O157:H7 in an unopened package of Ready Pac Bistro® Chicken Caesar Salad collected from an ill person’s home in Maryland. Analysis of this salad, through Whole Genome Sequencing (WGS), has linked strain E. coli O157:H7 to three Maryland cases and the multi-state outbreak.
The FDA and state partners are conducting a traceback investigation to trace romaine exposures to the source. Preliminary information indicates that ill people in Maryland were exposed to romaine lettuce harvested in Salinas, California.
FDA has deployed investigators to the farms in question to try to determine the source and extent of the contamination. More information will be forthcoming as the investigation proceeds.
Additionally, state partners are conducting laboratory analyses of romaine lettuce samples from case patients potentially linked to the outbreak.
The Salinas region as defined by the United Fresh Produce Association and the Produce Marketing Association Romaine Taskforce ReportExternal Link Disclaimer includes: Santa Cruz, Santa Clara, San Benito, and Monterey counties in California.
Genetic analysis of the E. coli O157:H7 strains from patients in this current outbreak are similar to strains of E. coli O157:H7 associated with a previous outbreak from the Fall of 2017 and the Fall of 2018 that affected consumers in both Canada and the U.S. The 2017 outbreak of E. coli O157:H7 was associated with leafy greens in the U.S. and romaine in Canada. The 2018 outbreak of E. coli O157:H7 was associated with romaine in both countries.
What Products are Recalled?
On Nov. 21, 2019, the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) announced a recall by Missa Bay, LLC, a Swedesboro, N.J. establishment, of approximately 75,233 pounds of salad products that contain meat or poultry because the lettuce ingredient may be contaminated with E. coli 0157:H7. Products in this recall were produced with the same lot of lettuce that was used to produce the packaged salad that the Maryland Department of Health found to contain E. coli 0157:H7.
The products subject to the recall can be found in a spreadsheet on the FSIS website. FSIS will likely update the poundage as more information becomes available. FSIS has posted product labels on its website.
The products subject to recall bear establishment number “EST. 18502B” inside the USDA mark of inspection. These items were shipped to distribution locations in Alabama, Connecticut, Florida, Georgia, Illinois, Indiana, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, New Jersey, New York, North Carolina, Ohio, Pennsylvania, South Carolina, Virginia and Wisconsin.
Consumers with questions regarding the recall can contact Mary Toscano, Consumer Affairs Manager for Bonduelle at 1-800-800-7822. Members of the media with questions regarding the recall can contact the Bonduelle Newsroom at (626) 678-2222 or bfa-newsroom@bonduelle.com.
What is E. coli?
E. coli are mostly harmless bacteria that live in the intestines of people and animals and contribute to intestinal health. However, eating or drinking food or water contaminated with certain types of E. coli can cause mild to severe gastrointestinal illness. Some types of pathogenic (illness-causing) E. coli, such as Shiga toxin-producing E. coli (STEC), can be life-threatening.
People infected with pathogenic E. coli can start to notice symptoms anywhere from a few days after consuming contaminated food or as much as nine days later. Generally, the symptoms include severe stomach cramps, diarrhea, fever, nausea, and/or vomiting.
The severity or presence of certain symptoms may depend on the type of pathogenic E. coli causing the infection. Some infections can cause severe bloody diarrhea and lead to life-threatening conditions, such as a type of kidney failure called hemolytic uremic syndrome (HUS), or the development of high blood pressure, chronic kidney disease, and neurologic problems. Other infections may have no symptoms or may resolve without medical treatment within five to seven days.
Due to the range in severity of illness, people should consult their health care provider if they suspect that they have developed symptoms that resemble an E. coli infection, including HUS, but even healthy older children and young adults can become seriously ill.
People of any age can become infected with pathogenic E. coli. Children under the age of 5 years, adults older than 65, and people with weakened immune systems are more likely to develop severe illness as a result of an E. coli infection. However, even healthy older children and young adults can become seriously ill.
General Food Safety Tips for Retailers
Restaurants and retailers should always practice safe food handling and preparation measures. It is recommended that employees wash hands, utensils, and surfaces with hot, soapy water before and after handling food.
•Regular frequent cleaning and sanitizing of food contact surfaces and utensils used in food preparation may help to minimize the likelihood of cross-contamination.
•Wash and sanitize display cases and refrigerators regularly.
•Wash and sanitize cutting boards, surfaces, and utensils used to prepare, serve, or store food.
•Wash hands with hot water and soap following the cleaning and sanitation process.
General Food Safety Tips for Consumers
People should consult their healthcare provider if they suspect that they have developed symptoms that resemble an E. coli infection.
Consumers should follow these steps for preventing foodborne illness:
•Wash the inside walls and shelves of the refrigerator, cutting boards and countertops, and utensils that may have contacted contaminated foods; then sanitize them with a solution of one tablespoon of chlorine bleach to one gallon of hot water; dry with a clean cloth or paper towel that has not been previously used.
•Wash and sanitize surfaces used to serve or store potentially contaminated products.
•Wash hands with warm water and soap following the cleaning and sanitation process.
Consumers can also submit a voluntarily report, a complaint, or adverse event (illness or serious allergic reaction) related to a food product.
According to the CDC, as of November 25, 2019, 67 people infected with the outbreak strain of E. coli O157:H7 have been reported from 19 states. The case patients report that illnesses started on dates ranging from September 24, 2019 to November 14, 2019.
The Maryland Department of Health identified E. coli O157:H7 in an unopened package of Ready Pac Bistro® Chicken Caesar Salad collected from an ill person’s home in Maryland. Analysis of this salad, through Whole Genome Sequencing (WGS), has linked strain E. coli O157:H7 to three Maryland cases and the multi-state outbreak.
The FDA and state partners are conducting a traceback investigation to trace romaine exposures to the source. Preliminary information indicates that ill people in Maryland were exposed to romaine lettuce harvested in Salinas, California.
FDA has deployed investigators to the farms in question to try to determine the source and extent of the contamination. More information will be forthcoming as the investigation proceeds.
Additionally, state partners are conducting laboratory analyses of romaine lettuce samples from case patients potentially linked to the outbreak.
The Salinas region as defined by the United Fresh Produce Association and the Produce Marketing Association Romaine Taskforce ReportExternal Link Disclaimer includes: Santa Cruz, Santa Clara, San Benito, and Monterey counties in California.
Genetic analysis of the E. coli O157:H7 strains from patients in this current outbreak are similar to strains of E. coli O157:H7 associated with a previous outbreak from the Fall of 2017 and the Fall of 2018 that affected consumers in both Canada and the U.S. The 2017 outbreak of E. coli O157:H7 was associated with leafy greens in the U.S. and romaine in Canada. The 2018 outbreak of E. coli O157:H7 was associated with romaine in both countries.
What Products are Recalled?
On Nov. 21, 2019, the U.S. Department of Agriculture’s Food Safety and Inspection Service (FSIS) announced a recall by Missa Bay, LLC, a Swedesboro, N.J. establishment, of approximately 75,233 pounds of salad products that contain meat or poultry because the lettuce ingredient may be contaminated with E. coli 0157:H7. Products in this recall were produced with the same lot of lettuce that was used to produce the packaged salad that the Maryland Department of Health found to contain E. coli 0157:H7.
The products subject to the recall can be found in a spreadsheet on the FSIS website. FSIS will likely update the poundage as more information becomes available. FSIS has posted product labels on its website.
The products subject to recall bear establishment number “EST. 18502B” inside the USDA mark of inspection. These items were shipped to distribution locations in Alabama, Connecticut, Florida, Georgia, Illinois, Indiana, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, New Jersey, New York, North Carolina, Ohio, Pennsylvania, South Carolina, Virginia and Wisconsin.
Consumers with questions regarding the recall can contact Mary Toscano, Consumer Affairs Manager for Bonduelle at 1-800-800-7822. Members of the media with questions regarding the recall can contact the Bonduelle Newsroom at (626) 678-2222 or bfa-newsroom@bonduelle.com.
What is E. coli?
E. coli are mostly harmless bacteria that live in the intestines of people and animals and contribute to intestinal health. However, eating or drinking food or water contaminated with certain types of E. coli can cause mild to severe gastrointestinal illness. Some types of pathogenic (illness-causing) E. coli, such as Shiga toxin-producing E. coli (STEC), can be life-threatening.
People infected with pathogenic E. coli can start to notice symptoms anywhere from a few days after consuming contaminated food or as much as nine days later. Generally, the symptoms include severe stomach cramps, diarrhea, fever, nausea, and/or vomiting.
The severity or presence of certain symptoms may depend on the type of pathogenic E. coli causing the infection. Some infections can cause severe bloody diarrhea and lead to life-threatening conditions, such as a type of kidney failure called hemolytic uremic syndrome (HUS), or the development of high blood pressure, chronic kidney disease, and neurologic problems. Other infections may have no symptoms or may resolve without medical treatment within five to seven days.
Due to the range in severity of illness, people should consult their health care provider if they suspect that they have developed symptoms that resemble an E. coli infection, including HUS, but even healthy older children and young adults can become seriously ill.
People of any age can become infected with pathogenic E. coli. Children under the age of 5 years, adults older than 65, and people with weakened immune systems are more likely to develop severe illness as a result of an E. coli infection. However, even healthy older children and young adults can become seriously ill.
General Food Safety Tips for Retailers
Restaurants and retailers should always practice safe food handling and preparation measures. It is recommended that employees wash hands, utensils, and surfaces with hot, soapy water before and after handling food.
•Regular frequent cleaning and sanitizing of food contact surfaces and utensils used in food preparation may help to minimize the likelihood of cross-contamination.
•Wash and sanitize display cases and refrigerators regularly.
•Wash and sanitize cutting boards, surfaces, and utensils used to prepare, serve, or store food.
•Wash hands with hot water and soap following the cleaning and sanitation process.
General Food Safety Tips for Consumers
People should consult their healthcare provider if they suspect that they have developed symptoms that resemble an E. coli infection.
Consumers should follow these steps for preventing foodborne illness:
•Wash the inside walls and shelves of the refrigerator, cutting boards and countertops, and utensils that may have contacted contaminated foods; then sanitize them with a solution of one tablespoon of chlorine bleach to one gallon of hot water; dry with a clean cloth or paper towel that has not been previously used.
•Wash and sanitize surfaces used to serve or store potentially contaminated products.
•Wash hands with warm water and soap following the cleaning and sanitation process.
Consumers can also submit a voluntarily report, a complaint, or adverse event (illness or serious allergic reaction) related to a food product.

No comments:
Post a Comment